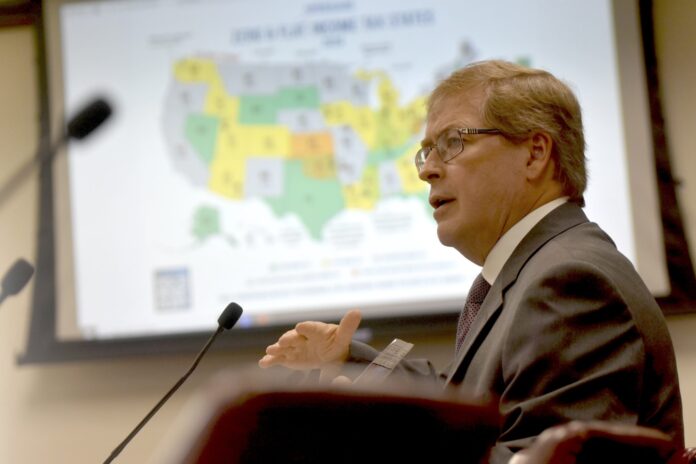
Insurance and Safety Fire Commissioner John F. King said Friday that Georgia will pay health insurance firms over $20 million for violating mental health parity standards.
In 2022, I witnessed the signing of Georgia’s Mental Health Parity Act into law. According to King, three years later, our preliminary investigations reveal that insurers have disregarded the regulations and are still denying Georgians the necessary behavioral health services they are entitled to.
According to the law, insurance companies must pay for mental health and drug addiction treatment on an equal footing with medical care. In order to verify compliance, state regulators examine data annually. Should issues arise, they have the authority to initiate comprehensive audits, also referred to as market conduct exams.
Over 6,000 infractions at 22 insurance companies were found during those assessments. Regulators pointed to problems such claims being reprocessed without apparent reason, uneven benefit classifications, and needless prior permission requirements.
King stated that yesterday was the deadline for complying with the law.
According to Georgia law, an insurer who knew or should have known it was infringing the law might face fines of up to $5,000 for each infraction. In addition to fines, businesses may be required to follow compliance plans or reprocess claims.
According to the Office of the Commissioner of Insurance, it will keep an eye on insurers to make sure they adhere to parity regulations. If a consumer feels they have been refused equal coverage, they can call 1-800-656-2298 or visit oci.georgia.gov to register a complaint.